 A recent study identified mixed viral populations in Pseudomonas aeruginosa (Pa) bacteria colonizing the lungs of patients with Cystic Fibrosis and non-Cystic Fibrosis bronchiectasis that may contribute to bacterial pathogenicity in the chronic lung. The study entitled “A metagenomic approach to characterize temperate bacteriophage populations from Cystic Fibrosis and non-Cystic Fibrosis bronchiectasis patients” was published in Frontiers in Microbiology by Mohammad A. Tariq and Francesca L. C. Everest, co-first authors, and Dr. Darren L. Smith, senior author, from the Faculty of Health and Life Sciences, University of Northumbria at Newcastle, Newcastle Upon Tyne, UK, along with colleagues.
A recent study identified mixed viral populations in Pseudomonas aeruginosa (Pa) bacteria colonizing the lungs of patients with Cystic Fibrosis and non-Cystic Fibrosis bronchiectasis that may contribute to bacterial pathogenicity in the chronic lung. The study entitled “A metagenomic approach to characterize temperate bacteriophage populations from Cystic Fibrosis and non-Cystic Fibrosis bronchiectasis patients” was published in Frontiers in Microbiology by Mohammad A. Tariq and Francesca L. C. Everest, co-first authors, and Dr. Darren L. Smith, senior author, from the Faculty of Health and Life Sciences, University of Northumbria at Newcastle, Newcastle Upon Tyne, UK, along with colleagues.
Chronic respiratory diseases are responsible for about 4 million deaths worldwide per year. Cystic Fibrosis (CF) is a rare but well described genetic chronic respiratory disease and is associated with chronic bacterial infections of the lung. Non-Cystic Fibrosis bronchiectasis (nCFBR) occurs normally in older populations and it is an abnormal and irreversible dilation of the lower bronchi. CF and nCFBR share the common feature of having similar susceptibility for Pseudomonas aeruginosa (Pa), an opportunistic pathogen, and atypical accumulation of mucus in the lower respiratory tract.
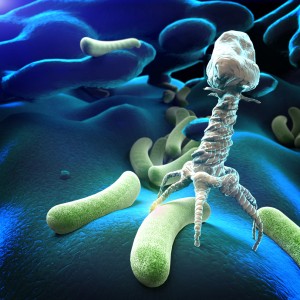
In this study, the researchers focused on temperate bacteriophages since they are an intrinsic part of the adaptation and evolution of bacteria. These phages have been shown to have a series of genes that can change the pathogenicity of a bacterium. Temperate bacteriophages upon entry into the bacterium integrate its genome as a prophage and stay dormant until they are induced and then originate an infective phage particle.
The authors hypothesized that temperate phages may use the mucus barrier, first line of defense for protection against pathogenic infection, in the lung as a way of infecting incoming bacteria leading to gene exchange between them and improve their adaptation and evolution. They wanted to address if the Bacteriophage Adherence to Mucus (BAM) model could be applied to temperate bacteriophages. This model proposes that lytic phages, other class of phages, adhere to carbohydrate residues present inside the mucus layer and provide a cover of immunity to incoming bacteria. For this, they compared the inducible temperate phages of Pa found in the lungs of patients with CF and nCFBR using for the first time a metagenomic approach, a method of sequencing and analysis of DNA from a mixed population of microorganisms.
This study gave the first indication of the complexities of the phage genomes and how they may adapt over time and obtain accessory genes associated with key metabolic and signaling processes that favor phage survival and bacterial pathogenicity in the chronic lung. With the increasing concerns about microbial resistance the temperate phages may be a potential target to fight resistance and persistence pathways of bacteria.

