In a new study entitled “A randomised, placebo-controlled study of the CXCR2 antagonist AZD5069 in bronchiectasis”, researchers performed a randomized, double-blind, placebo-controlled study to determine the effect of CXCR2 antagonist AZD5069 on sputum neutrophil counts in adults with bronchiectasis. The study was published in the European Respiratory Journal.
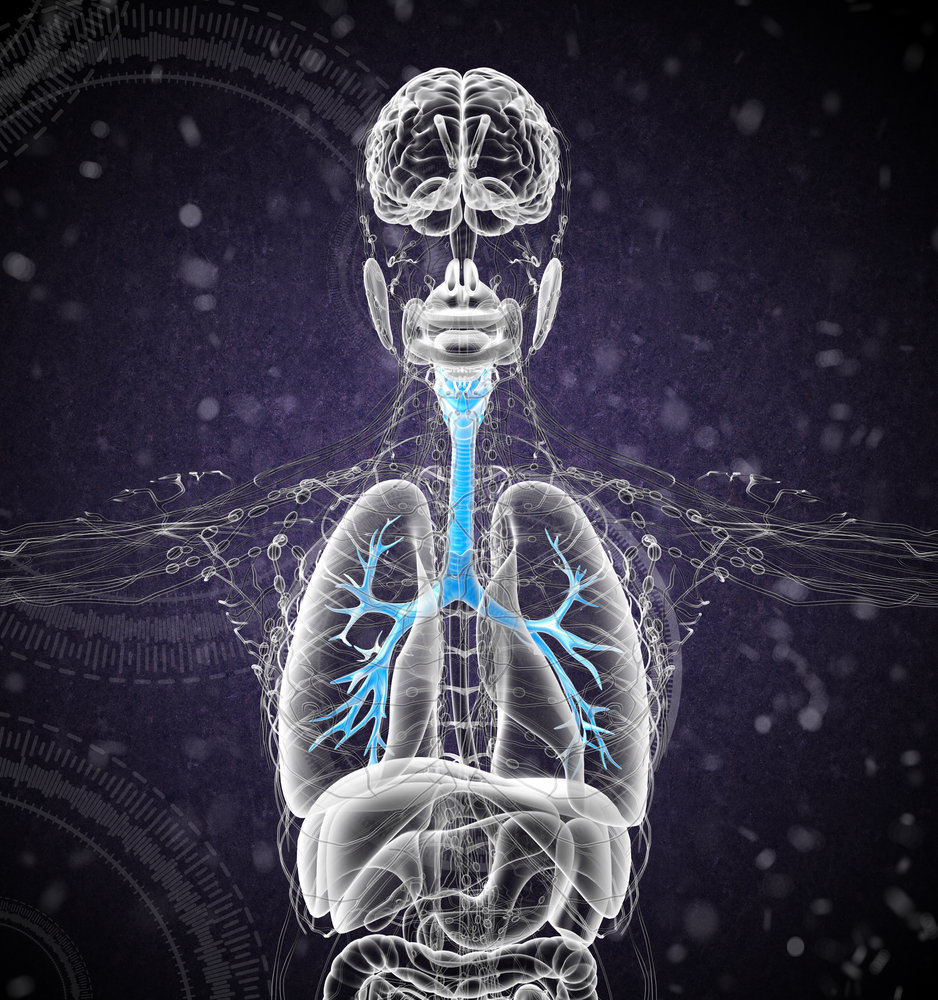
Bronchiectasis is a condition characterized by a permanent abnormally widening and damage of the bronchial tubes. The condition is often caused by an infection that damages the walls of the lungs’ airways or prevents the clearing of mucus, a substance produced by the lungs to remove foreign particles (dust or bacteria). In bronchiectasis patients, the ability to remove mucus from airways is impaired resulting in mucus accumulation, fostering the growth of bacteria. This leads to continuous lung infections, which trigger the recruitment of immune cells.
Neutrophils, the most abundant type of white blood cells, are the dominant cells present in mucus from bronchiectasis patients, recruited to defend the organism against bacterial infection. Once in the airways, however, the massive recruitment of neutrophils induces epithelial damage to lung cells and increases the secretion of mucus.
Here, authors performed a randomized double-blind, multicentre phase IIa study to determine the potential inhibitory effect on neutrophil recruitment of the CXC-chemokine receptor 2 (CXCR2) antagonist called AZD5069 (previous studies in patients with chronic obstructive pulmonary disease showed CXCR2 antagonist reduced sputum neutrophils). CXCR2 is important in controlling the extravasation and activation of neutrophils.
To this end, patients with bronchiectasis were randomly assigned to received either AZD5069 (80 mg) or a placebo control, in a twice a day regiment for 28 days. The effect of AZD5069 was determined by measuring blood cells, presence of inflammatory markers in the blood, morning spontaneous sputum and lung function. Additionally, the team determined the safety and tolerability of the drug.
The team observed that AZD5069 reduced the absolute neutrophil cell count in morning sputum by 69% when compared to the placebo control group, and that the drug was well tolerated by the patients. However, despite AZD5069 markedly reduced absolute sputum neutrophil counts in bronchiectasis patients, the team of authors observed no improvement on clinical outcomes of bronchiectasis patients treated with AZD5069.