An allergic reaction to mold may increase the risk of people with COPD developing bronchiectasis, a disorder that involves damaged lung airways, according to researchers in Belgium.
The team at University Hospitals Leuven and KU Leuven reported that antibodies against the common mold Aspergillus (A.) fumigatus were much more common in COPD patients than in healthy people. They also reported a connection between the mold and bronchiectasis.
They noted that their study was retrospective, however — that is, based on previous medical records. A study that looks for a cause-and-effect relationship is needed to prove that the mold actually triggers bronchiectasis, the team said.
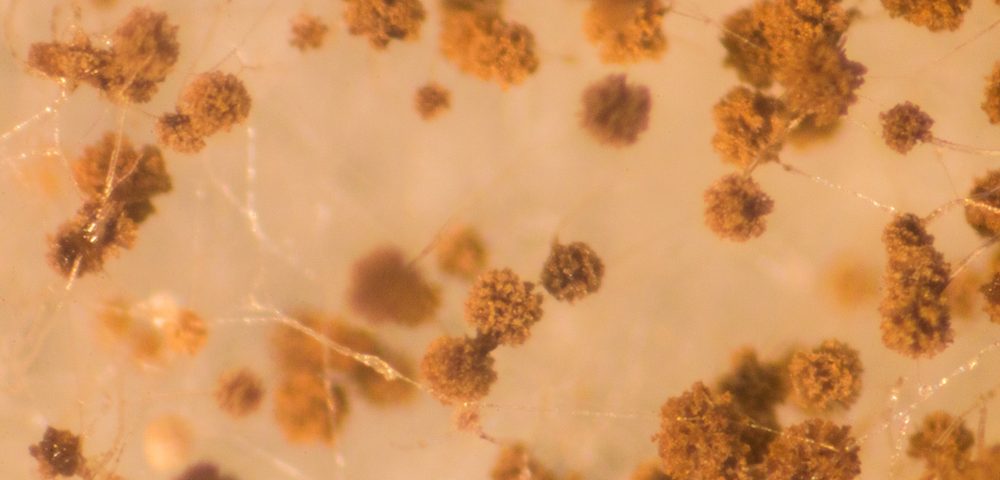
A. fumigatus is common in our environment, and the immune system of healthy people can usually handle the inhaled intruder. The immune system of COPD patients can be compromised, however.
Researchers published the study, “Sensitization to Aspergillus fumigatus as a risk factor for bronchiectasis in COPD,” in the International Journal of Chronic Obstructive Pulmonary Disease.
The team recruited 300 COPD patients from an outpatient clinic for their study. The patients were already enrolled in a clinical trial (NCT00858520) that was collecting samples of their DNA, blood and tissue.
Researchers also recruited 50 controls who were either current or former smokers, and who were part of another study.
As the team suspected, a lot more COPD patients than controls had antibodies indicating they had had allergic reactions to A. fumigatus. In fact, 18 percent of the COPD patients had the antibodies, versus 4 percent of the controls. The proportion of people with bronchiectasis was also higher among COPD patients than among controls.
The team found no link between A. fumigatus and body mass index, smoking history, or use of inhaled corticosteroids.
Another finding was that antibodies to A. fumigatus were more common in men and in those with bronchiectasis. Two specific antibodies turned out to be most closely linked to bronchiectasis. All who had them had the damaged airway condition.
Interestingly, patients who showed signs of being allergic to the mold did not have more COPD exacerbations than non-allergic patients. And the two groups had similar lung function impairment and COPD severity.
When researchers looked at sputum samples, they discovered that COPD patients with antibodies against A. fumigatus had more harmful microbes in their airways. These consisted mostly of the bacteria Pseudomonas aeruginosa and Serratia marcescens.
Additional analysis revealed that age, A. fumigatus antibodies, and bronchiectasis were closely linked in COPD patients.
“Because of the retrospective, observational design of this study, we were not able to demonstrate a causal relationship” between the mold and bronchiectasis, the team wrote. Still, the study was the first linking the two in COPD patients, they wrote.
“The search for underlying mechanisms in the development of bronchiectasis in COPD is relevant, since the presence of bronchiectasis in COPD influences management and prognosis of the disease,” they wrote. “Prospective, longitudinal studies are needed to prove causality and to allow speculation about preventive interventions.”