An analysis of previously published studies revealed that patients with chronic obstructive pulmonary disease (COPD) who also suffer from bronchiectasis have a higher risk of exacerbation and worse outcomes. The results indicated that clinical vigilance is crucial, since COPD patients with bronchiectasis might benefit from specific therapies.
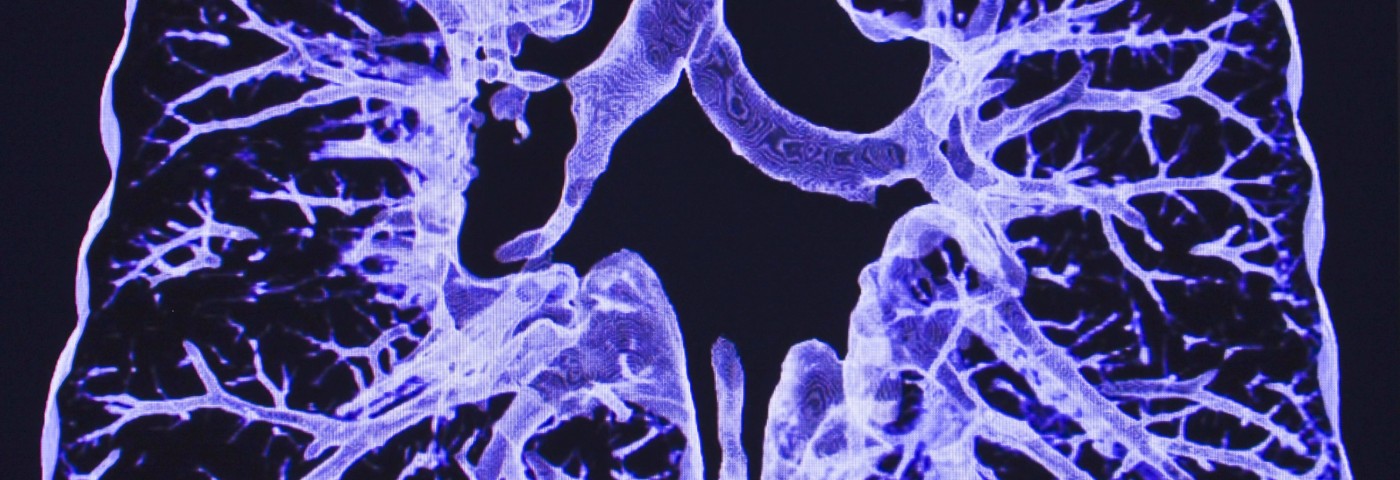
While COPD is in itself one of the leading causes of death in the world, underlying airway structural changes, such as bronchiectasis, might further complicate the condition. The two conditions share clinical features, such as the presence of a chronic cough, high sputum production, and an airflow obstruction that is not possible to fully reverse.
Researchers from Capital Medical University in Beijing, China, noted that many studies reported that COPD patients with confirmed bronchiectasis had increased airway inflammation, frequent infections with potentially pathogenic microorganisms, and more severe airflow obstruction. There were, however, also studies finding no relationship between the conditions in terms of worse outcomes.
The study, “Bronchiectasis as a Comorbidity of Chronic Obstructive Pulmonary Disease: A Systematic Review and Meta-Analysis,“ published in the journal PLOS ONE, analyzed data from published studies to see if these associations would hold.
The researchers observed that COPD-bronchiectasis patients had nearly twice as high a risk of exacerbations, compared to COPD patients without bronchiectasis. Also, the risk of being infected with a potentially pathogenic microorganism was almost four times higher for these patients.
Four studies included in the analysis looked specifically at Pseudomonas aeruginosa infections, which seemed to be even more common in this patient group than other infections, but the results of the included studies were highly variable. Findings concerning severe airway obstruction and a higher mortality risk also varied across studies. Despite the variability, the analysis showed an increased risk for worse airway obstruction and death.
The authors argued that the vastly varying findings can be tied to the clinical heterogeneity of the various study settings and included patients.
Since the researchers found evidence of publication bias – the tendency to only publish confirmatory results – they performed a simulation to see how the results of the analysis would change if also hypothetical negative studies were included. They noted that the association between bronchiectasis in COPD and worse outcomes was still valid even after balancing the results with theoretical negative studies.
Given the results obtained, more research on how bronchiectasis in COPD affects the patient clinical management is urgently needed, particularly in exploring specific therapies that might be beneficial for this group of patients.