A newly developed fluorescent probe allows the detection of infectious bacteria in human airways and lung’s air sacs within minutes, a study shows.
This innovative diagnostic strategy was found to be safe and easy to use in humans, enabling early diagnosis and treatment of potentially serious pulmonary infections.
Developed by researchers at the University of Edinburgh, the diagnostic tool was described in a study titled “In situ identification of Gram-negative bacteria in human lungs using a topical fluorescent peptide targeting lipid A,” published in the journal Science Translational Medicine.
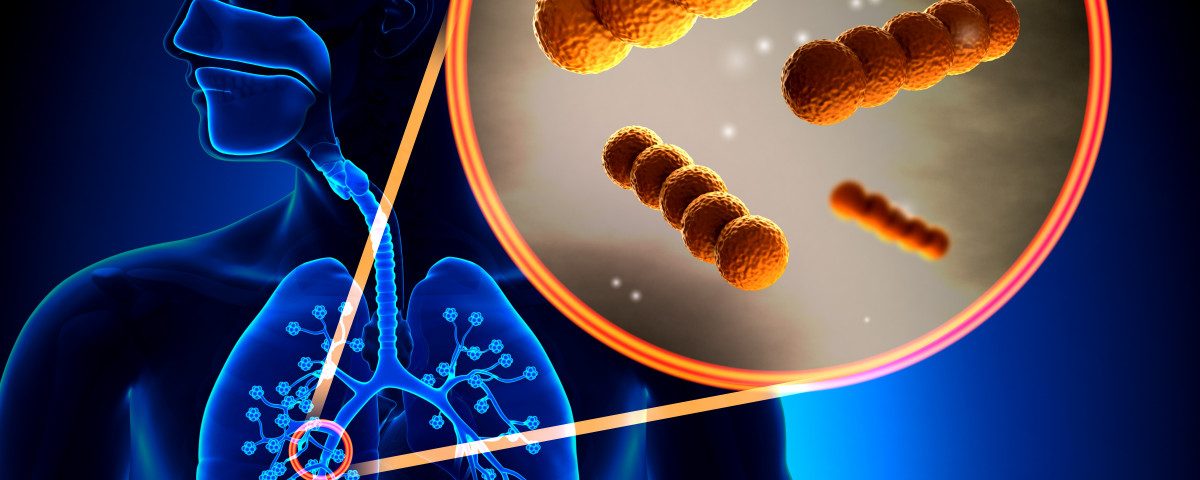
Gram-negative bacteria, such as Pseudomonas aeruginosa and Escherichia coli, are the main culprits for serious, drug-resistant infections, which are particularly frequent among patients with a debilitated immune system, pulmonary diseases such as bronchiectasis, or under mechanical ventilation.
Diagnosis of lung bacterial infections and treatment selection currently relies on the analysis of aspirated fluids or expectorated samples along with antimicrobial susceptibility testing.
But this approach has several limitations. The collected samples may not provide a full representation of the bacterial load present in the lungs, or may be contaminated with other bacteria strains present in the trachea or mouth, failing to accurately identify the cause of the infection and leading to over-treatment with antibiotics.
To overcome these limitations, researchers developed a new probe that could efficiently help detect bacteria in the lungs.
They used a small bacteria-derived protein called polymyxin, or PMX, that can bind to the toxic lipopolysaccharide (LPS) molecule present in the outer membrane of Gram-negative bacteria. By combining PMX with a fluorescent probe, the team could easily track bacteria in an experimental setting.
To further explore the potential of this new diagnostic probe, the team tested it in a ventilated sheep lung model. Researchers confirmed they could efficiently visualize in real time — with an optical fiber inserted inside the lungs — the infectious bacteria, while the not dangerous bacteria (Gram-positive bacteria) were not labeled by the fluorescent probe.
After ensuring the probe was generally stable and not toxic for human tissues, the team tested it in patients with bronchiectasis and in patients mechanically ventilated in an intensive care unit.
The probe was applied topically as a micro-dose through an intrapulmonary catheter during a bronchoscopy procedure to six bronchiectasis and seven ventilated patients. The visualization procedure was begun immediately after the probe was administered.
Using a computer-based analysis method designed specifically for this probe, the team could efficiently differentiate between Gram-negative and Gram-positive bacteria present in the lungs of patients. In particular, with this approach, they could detect the presence of infectious bacteria in the lungs’ air sacs, which are commonly considered to have a low bacterial load.
The positive bacterial results collected with the probe were further confirmed upon analysis of the patient’s bacterial burden with conventional diagnosis methods.
With this new approach, the team showed that it is possible to “delineate bacterial presence in distinct segments of the pulmonary tree,” they said. “The specificity, safety, and rapid readout of this technology platform represent potentially significant advantages over current technologies and now require further large-scale validation.”
Minor adverse events, such as a cough attributable to the bronchoscopy procedure, were observed in three bronchiectasis patients, and no serious adverse events were reported in ventilated patients.
“Drug-resistant bacteria are fast emerging as the greatest threat to humanity,” Kev Dhaliwal, MD, PhD, professor at the University of Edinburgh, consultant respiratory physician, and senior author of the study, said in a university press release.
“The teamwork required to deliver this bench to bedside technology has taken many years and we are incredibly grateful to the patients and families who allowed us to test these exciting approaches and now the follow-on funding to further develop and test this technology in intensive care units around the U.K.,” Dhaliwal added.
The team believes this technology could help doctors in decision-making processes regarding treatment and avoid unnecessary antibiotic use.