A retrospective study of acute eosinophilic pneumonia (AEP) patients found that traction bronchiectasis (TBE) may be associated with a poor prognosis and fatal AEP.
The study, “Traction bronchiectasis on high-resolution computed tomography may predict fatal acute eosinophilic pneumonia,” was published in the journal Respiratory Investigation.
AEP is rare, often with rapid onset of symptoms (one to seven days) characterized by an accumulation of eosinophils in the lungs. Eosinophils are a type of immune cells that can be activated by allergens, inflammation or infections, and can cause low levels of oxygen in the blood and subsequent respiratory failure.
Bronchoalveolar lavage (BAL) is the main method of diagnosing AEP. By inserting a narrow tube into the windpipe, washing out and collecting the cells lining the tissue, clinicians can study the cell composition in the lungs and detect abnormal levels of eosinophils (greater than 25%).
Patients with AEP generally respond well to corticosteroid treatment. Still, the disease course can vary widely, ranging from quick improvement to a life-threatening situation.
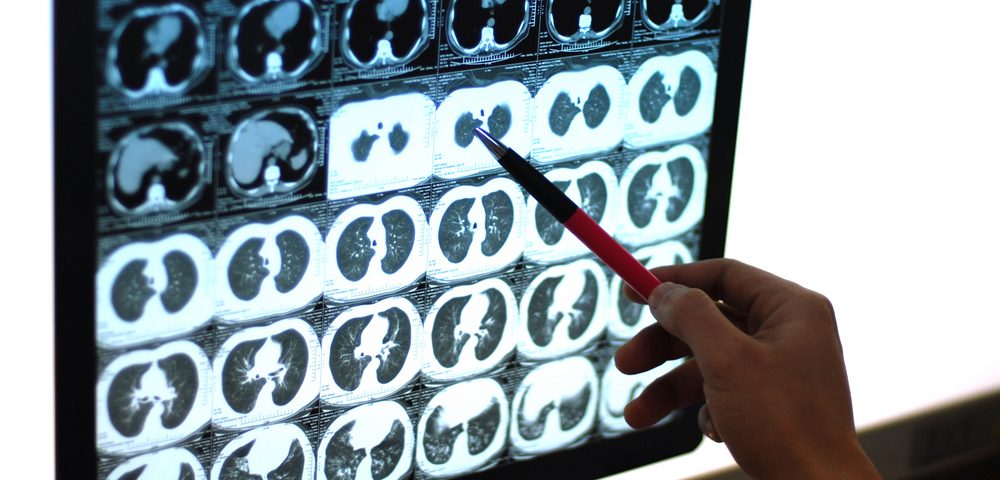
To further understand the disease and its predicted course, researchers investigated potential signs of poor prognosis by assessing AEP patients’ clinical, radiographic, and pathological characteristics. TBE (structural changes in the airways associated with fibrosis) was assessed through high-resolution computed tomography (HRCT).
Researchers compared 2005-2013 medical records from the Kurashiki Central Hospital in Japan. These contained clinical data from 41 patients (median age 66) diagnosed with AEP. Patients were included in the study if the data indicated acute onset of respiratory symptoms of AEP lasting less than one month, lung infiltrates, and accumulation of eosinophils (median percentage among patients was 51% as measured by BAL).
AEP patients were categorized into three groups, depending on the disease cause: idiopathic (of unknown cause), medical-related, and smoking-related AEP.
Results showed that of the six smoking-related AEP patients in the study, none had signs of TBE and they responded to corticosteroid treatment better than idiopathic or medication-related AEP patients. Overall, smoking-related AEP patients had a better prognosis, with shorter hospitalization and treatment duration, and no reported deaths.
Four of the 41 patients with AEP analyzed died after not responding to corticosteroid treatment (mean survival after diagnosis 17 days). While three of the fatal AEP cases were idiopathic, one was medication-related. Patients with fatal AEP had a median eosinophil percentage of 59%, based on BAL.
All four people who died had been diagnosed with TBE, according to HRCT results. Because no TBE had been confirmed before AEP diagnosis, researchers suggested that the condition was secondary to AEP.
Six of the 41 patients had TBE. Of the two surviving AEP patients with TBE, one showed no signs of fibrosis (scarred tissue) and one showed signs of fibrosis that persisted after corticosteroid-associated improvement of AEP.
Overall, although the patient number analyzed was small, the results suggest that certain characteristics, namely TBE, are associated with worse AEP outcome.
“TBE was observed in all fatal cases and may be associated with a poor prognosis,” the researchers stated.
“Although it is difficult to identify the true onset of AEP, considering that it is before the appearance of symptoms, it seems likely that TBE would be seen at the initial HRCT evaluation,” the researchers said. Therefore, “TBE on initial HRCT may be an important change heralding the start of fibrosis, which is a poor prognostic factor in AEP.”
The team concluded that “more patients similar to those who died in our study should be investigated to identify more appropriate treatment methods for AEP.”