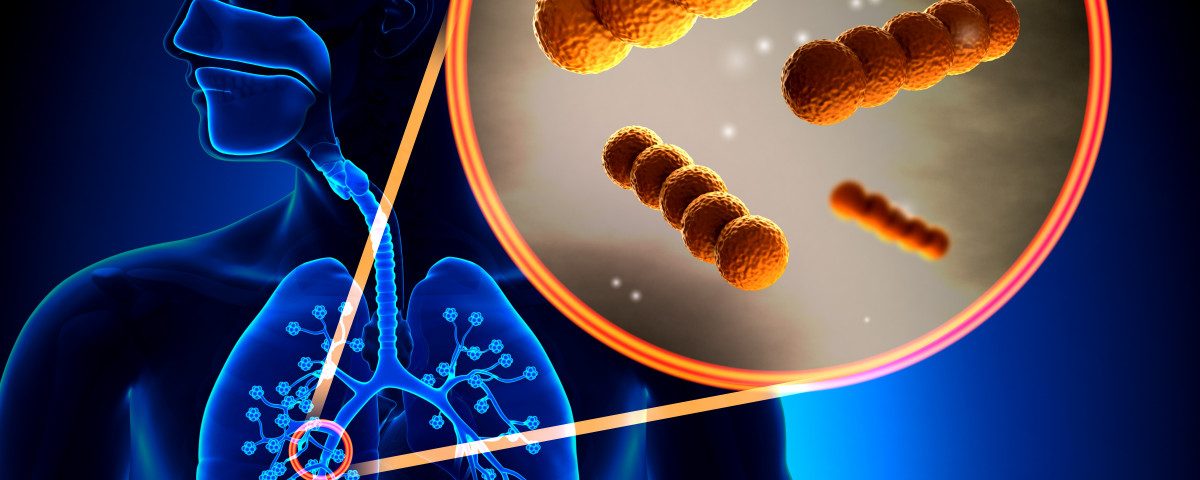
Pseudomonas aeruginosa, the most common bacterial infection found in bronchiectasis patients, can adapt in the lungs and acquire a mucoid state that makes sputum harder to clear, new research shows. Bacteria that mutate in this way are also linked to more severe disease.
The study, “Mucoid Pseudomonas aeruginosa alters sputum viscoelasticity in patients with non-cystic fibrosis bronchiectasis,” was published in the journal Respiratory Medicine.
Mucus that lubricates the bronchi — the conducting airways — is produced and expelled continuously, but in people with bronchiectasis an excessive production and changes in the mucus’ mechanical properties make it harder to clear. This creates the perfect conditions for infections, of which the bacteria Pseudomonas aeruginosa is one of the most common.
Mutations in the gene mucA in P. aeruginosa make the bacteria transition from a non-mucoid to a mucoid state that is characterized by an excessive production of the exopolysaccharide alginate. Alginate is used by the bacteria to form biofilms — in which bacteria grow as a ‘community’ attached to a surface — a feature that contributes to the establishment of chronic infections.
Researchers in Spain investigated how non-mucoid and mucoid P. aeruginosa affect the viscosity and elasticity of mucus, and ultimately how it impacts clinical outcomes in bronchiectasis patients.
The team analyzed a total of 48 sputum (mucus) samples: 17 from bronchiectasis patients with mucoid P. aeruginosa, 14 from those with non-mucoid bacteria, and 17 from patients with no bacterial infection.
To measure sputum viscoelasticity, researchers used a technique called rheology that uses mechanical forces to detect changes in behavior.
Elasticity is the mechanical property that measures the tendency of a material to return to its original form after being deformed, while viscosity measures how much the material resists the tendency to flow. Hence, mucus with a high viscosity and low elasticity is more likely to remain intact and not move when air at high velocity passes through it.
Researchers found that, compared with infection-free patients, those with mucoid P. aeruginosa showed a tendency to have higher sputum viscosity (median 2.40 vs. 1.5 1rad/s), elasticity (median 10.30 vs. 5.70 1rad/s), and stiffness (median 10.70 vs. 6.0 1rad/s).
This trend might explain why patients with mucoid bacteria had more exacerbations or flares, and more pus (purulence) in their sputum than patients without infection.
Patients with chronic colonization with mucoid bacteria also had worse lung function, a higher level of dyspnea (shortness of breath), and more severe disease.
The team concluded that mucoid P. aeruginosa bacteria are “associated with increased elasticity, viscosity, and stiffness of bronchiectatic sputum” that “correlated with worse severity outcomes.”
Sputum “viscoelasticity assessment with rheology could be a new clinical tool in order to optimize and personalize bronchiectasis management,” and used “as a marker of poor mucociliary clearance,” the researchers added, noting that further studies are needed to confirm these findings.