Treatment with inhaled therapy Molgradex (molgramostim) stopped the growth of nontuberculous mycobacteria (NTM) in the sputum of bronchiectasis patients with chronic bacterial lung infections, according to topline results from a Phase 2a clinical trial.
However, safety analysis revealed that almost half the participants experienced serious side effects, the most common of which was exacerbation of bronchiectasis.
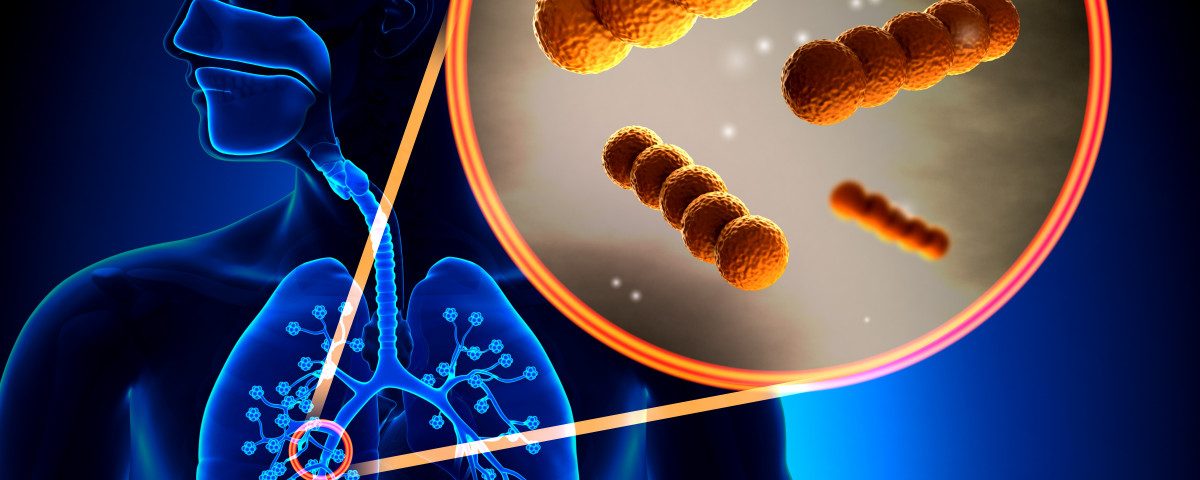
Lung infections caused by NTM are a considerable therapeutic challenge due to the unique ability of these bacteria to evade the normal killing mechanisms of alveolar macrophages, a type of immune cell responsible for killing bacteria in the lungs’ tiny air sacs (alveoli). These infections often becomes chronic and require prolonged treatment regimens, which are not always successful.
Savara Pharmaceuticals’ Molgradex is an inhaled, granulocyte-macrophage colony-stimulating factor (GM-CSF) that works by altering the body’s immune response to prevent the buildup of harmful bacteria in the lungs.
The OPTIMA trial (NCT03421743) assessed Molgradex’s safety and effectiveness. In this multicenter, pilot study, bronchiectasis patients with either Mycobacterium avium complex (MAC) infection or the more difficult-to-treat Mycobacterium abscessus (MABSC) infection underwent a 48-week treatment with Molgradex, with a 12-week follow-up. All patients had either antibiotic-resistant infection or intolerance to standard NTM antibiotics. No participant had cystic fibrosis (CF).
Thirty-four people were divided into two groups. Group 1 consisted of people with infections while on a standard anti-mycobacterial regimen for at least six months prior to study initiation.
Group 2 also included patients with infections, but they had either stopped a multi-therapy standard regimen at least 28 days prior to screening (due to lack of response or intolerance) or never started such treatment.
Twenty-four participants had MAC, and eight had MABSC infection. Among those with MAC infection, 11 were in group 1 and 13 were in group 2. Three patients with MABSC infection were in group 1, and five were in group 2.
Both groups received once daily inhaled Molgradex at a 300 µg dose.
OPTIMA’s primary goal was achieving sputum culture conversion following the 48-week treatment, which scientists defined as at least three consecutive sputum samples without growth of NTM.
Five patients (21%) with MAC infection achieved this goal. Two of them (one from each group) remained without NTM growth through the 12-week follow-up period, according to a press release.
No patient with a MABSC infection achieved such benefit, suggesting that Molgradex could be more effective in those with MAC infection.
In terms of safety, 14 participants experienced serious side effects, one of which considered potentially treatment-related. The most common serious adverse effect was exacerbation of bronchiectasis.
Three patients died during the course of the trial, but their deaths were likely unrelated to Molgradex, the company said.
Savara intends to present OPTIMA’s full results at an upcoming scientific conference.
Molgradex is also in Phase 2a development for NTM lung infection in CF-affected individuals (NCT03597347) and in Phase 2/3 for autoimmune pulmonary alveolar proteinosis (aPAP; NCT02702180). According to Savara, the study in aPAP, IMPALA, showed continued improvement in lung function and exercise capacity after 72-week treatment with Molgradex.