Adults with non-cystic fibrosis bronchiectasis (NCFBE) who were given brensocatib in a Phase 2 trial were 72% less likely to be at risk of an exacerbation if neutrophil elastase in their sputum fell to undetectable levels during treatment, data from a new analysis of this clinical study’s results indicate.
These findings were presented at the American Thoracic Society 2020 Virtual by James Chalmers, PhD, a trial investigator and University of Dundee professor. The presentation was titled, “Phase 2 Randomized Controlled Trial of DPP1 Inhibitor Brensocatib (INS1007) in Patients with Bronchiectasis: the WILLOW Study.”
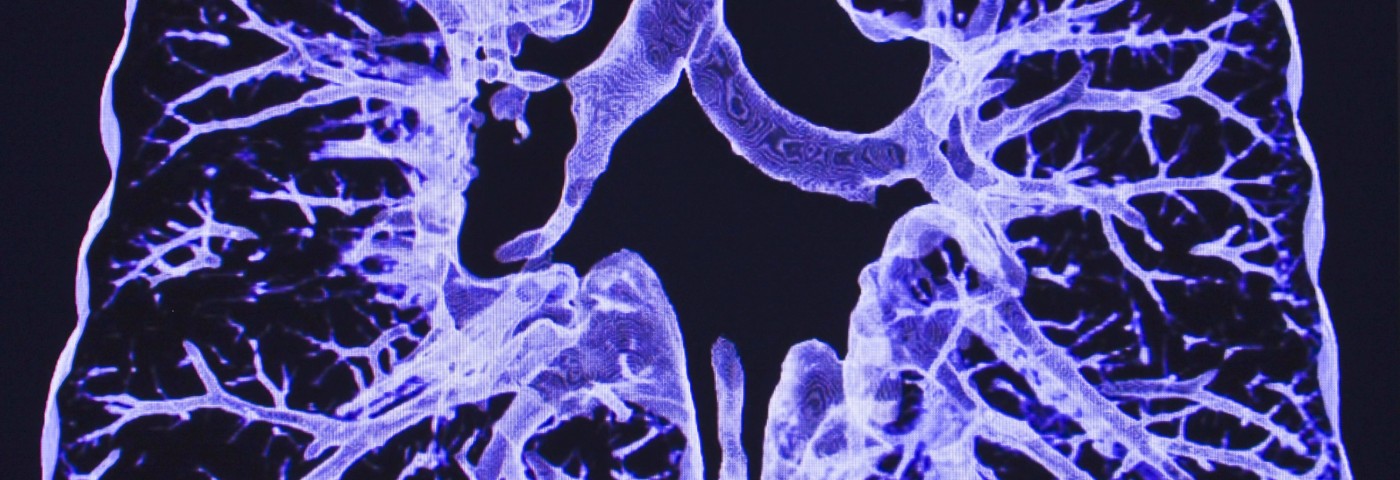
Brensocatib (formerly INS1007) is an oral small molecule that is intended to reduce the activity of neutrophils, a type of immune cell that helps drive inflammation in bronchiectasis. Reducing neutrophil activity is expected to lessen inflammation and damage to the lungs, ultimately leading to fewer bronchiectasis exacerbations.
The investigational therapy was recently designated a breakthrough therapy by the U.S. Food and Drug Administration. It is also being investigated as a possible treatment for COVID-19.
The Phase 2 WILLOW trial (NCT03218917) enrolled 256 adults with NCFBE who had at least two documented exacerbations in the past year. They were randomly assigned to one of two daily doses of brensocatib — 10 mg or 25 mg — or to a placebo for 24 weeks (six months).
Top-line results from WILLOW showed that the trial met its primary goal, with both brensocatib doses significantly delaying the time to a first bronchiectasis exacerbation. Both doses also significantly reduced the risk of an exacerbation at any time — by 42% for the 10 mg dose, and 38% for 25 mg.
Patients on brensocatib at 10 mg experienced a significant reduction, by 36%, in the rate of exacerbations — a key secondary measure. Those treated at 25 mg showed a trend toward a lower exacerbation rate, but the findings failed to reach statistical significance.
“I am very encouraged by the results from the Phase 2 WILLOW study, which underscore the potential for brensocatib to reduce the risk of pulmonary exacerbation in patients with NCFBE,” Chalmers said in a press release from Insmed, which acquired rights to brensocatib in 2016.
“These findings are critically important given the vicious cycle of inflammation, lung damage, and infection that patients with NCFBE face and the current lack of approved pharmaceutical therapies,” he added.
In addition to these previous findings, the recent presentation included data from an analysis of active neutrophil elastase — a protein associated with inflammation and lung damage — in patients’ sputum.
Neutrophils secrete this protein to fight threats like bacteria. However, neutrophil elastase can also damage healthy tissue, and is thought to play a central role in inflammatory lung damage in bronchiectasis. Measuring active neutrophil elastase, for this reason, can provide insight into the inflammatory activity of neutrophils in the lungs.
Patients given brensocatib at any dose were found to have significantly greater reductions in active neutrophil elastase than did those on placebo. And those who attained undetectable levels of neutrophil elastase after starting treatment with brensocatib were at 72% lower risk of an exacerbation, compared with patients with still detectable levels of this protein.
“We are thrilled to share positive final results from the Phase 2 WILLOW study today, confirming the top-line results presented earlier this year,” said Martina Flammer, MD, chief medical officer of Insmed. “Importantly, the new data presented today demonstrate the relationship between NE [neutrophil elastase] reduction and risk of exacerbation and serve as further proof of concept of the potential of brensocatib and its unique mechanism of action.”
Brensocatib was generally well tolerated in WILLOW. The most common adverse events in treated patients were cough, headache, increased sputum production, shortness of breath, exacerbations due to infection, diarrhea, fatigue, and upper respiratory tract infection (colds).
Adverse events leading to discontinuation occurred in 10.6% of participants on placebo, 7.4% of patients given 10 mg brensocatib, and 6.7% of those on the 25 mg dose.
Insmed is now planning a Phase 3 clinical trial of brensocatib in bronchiectasis patients.
“We look forward to initiating our Phase 3 program in bronchiectasis while also exploring the potential of brensocatib in other neutrophil-driven inflammatory conditions,” Flammer said.